There is a well-documented knowledge gap between healthcare providers and their transgender clients. Trans clients often have to adopt the role of educator and advocate in order to access the standards of care that their cisgender counterparts do. Due to the highly gendered historical approach to health, healthcare funding, and specifically sexual health, critical opportunities for screening, prevention, and treatment may be missed.
This information has been shared to provide sexual health considerations specifically for trans and gender diverse people to make informed decisions about their overall sexual health and wellbeing.
Libido (Sexual Desire)
While it is widely accepted that testosterone increases libido, one’s desire to be sexual or have sex has many factors besides hormone levels. When people are able to access transition-related care and experience more embodied gender euphoria, libido may reasonably increase. Being with a partner who practices consent and is affirming is also an important factor in libido and desire to have sex.
Sexual Health Considerations While Taking Hormones
- Testosterone can cause varying degrees of vaginal dryness and atrophy. This dryness and atrophy can predispose people to contracting STBBIs
- For this, a water-soluble lube is recommended
- Even though menses stop after taking testosterone, the ability to conceive remains
- Estrogen can reduce erections, but increase fluid secretions
- Medications for erectile dysfunction can be helpful
- Being on hormonal therapy does not mean there are no chances of pregnancy. Condoms and other methods of contraception are recommended.
Sexual Health Considerations after Transition-Related Surgeries
- It’s recommended that skin-lined vaginas (neovaginas) created by surgery be douched regularly
- Neovaginas do require regular dilation to maintain the shape and depth that allows for penetrative sex
- Metoidioplasty can sometimes but not always allow for penetrative sex
- After phalloplasty, penetrative sex is possible with implanted erectile devices or penis sleeves
STBBIs & Testing
Sexually transmitted and blood-borne infections (STBBIs) can be contracted during sex. STBBIs can be prevented through use of condoms, pre-exposure prophylaxis (PrEP), doxycycline post-exposure prophylaxis (doxy-PEP), and HIV post-exposure prophylaxis (PEP). Regular screening and treatment via STBBI clinics and in some cases, at-home dried blood/urine tests (also known as point-of-care tests, POC tests, or POCT) also assist in protection. Common STBBI symptoms include rashes, painful lumps, burning while peeing, and abnormal discharge. However, some infections are much more subtle and hard to detect.
If you suspect you have an STBBI, the best thing to do is visit your local STBBI clinic. Here are some options:
Calgary: Age 29 and Under
- Alberta Health Services Sexual and Reproductive Health Clinics
- Youth Clinic
- STI Clinics at Sheldon Chumir and East Calgary Health Centre
- Centre for Sexuality (ages 14+, all orientations and identities)
- The Alex Youth Health Centre (ages 12-24)
- Mosaic PCN Women’s Clinic
- University of Calgary and Mount Royal University offer health services for their students.
- Walk-in clinics or family doctors can also order testing. Clients need to get their lab requisition from a physician, then go to a lab afterwards to get the tests done.
- Centre for Sexuality offers STI testing just for gay, bisexual and other men who have sex with men.
Calgary: Age 29 and Over
- Alberta Health Services STI Clinics at Sheldon Chumir and East Calgary Health Centre
- Centre for Sexuality (ages 14+, all orientations and identities)
- Mosaic PCN Women’s Clinic
- University of Calgary and Mount Royal University offer health services for their students.
- Walk-in clinics or family doctors can also order testing. Clients need to get their lab requisition from a physician, then go to a lab afterwards to get the tests done.
- Centre for Sexuality offers STI testing just for gay, bisexual and other men who have sex with men.
Edmonton
- 24-Hour STI/HIV Information Line: 8-1-1
- Edmonton General Continuing Care Centre
- HIV Edmonton
- Compass Centre for Sexual Wellness
- Pride Centre of Edmonton
- Offers STI testing on every second and fourth Wednesday of the month.
- Steamworks (outreach office on the lower floor)
- STI testing every Tuesday and Thursday from 1-4pm. This testing is specifically catered towards men who have sex with men (MSM).
- Walk-in clinics or family doctors can also order testing. Clients need to get their lab requisition from a physician, then go to a lab afterwards to get the tests done.
- You can learn more about accessing STBBI testing in Edmonton here: https://ourhealthyeg.ca/sti-testing
Common tests at STBBI clinics are visual inspection, blood draws, urine samples, and swabs of the throat, rectum, and vagina. Vaginal swabs may not be undertaken routinely for people who have skin-lined vaginas/vaginoplasty, as emerging research does not support it. You can always request the presence of another staff member or trusted friend when accessing STBBI testing.
Testing is recommended before the start of a new sexual relationship, and every 3-6 months thereafter. For people who have sex without protection, testing every three months is reasonable. The window period of many common STBBIs mean that certain infections remain undetectable for months.
Condoms
Condoms are technically a medical device designed to provide a fluid barrier between two people during penetrative sex with a penis. Condoms are considered the best way to avoid not only STBBIs, but also unwanted pregnancies. Latex condoms can break down when used with oil-based lubricants, while water-based lubricants will maintain their integrity. It is recommended to always check the specific condom’s instructions or packaging for proper usage.
HIV Prevention
HIV is a virus that can weaken your immune system, your body’s built-in defence against disease and illness. Symptoms can be flu-like, such as fatigue, fever, sore throat, swollen lymph nodes, headache, loss of appetite, or a skin rash when HIV is first contracted. However, people can have HIV for a long time without any obvious symptoms. HIV can only be transmitted through these five body fluids:
- Blood
- Semen (including pre-cum)
- Rectal fluid
- Vaginal (frontal) fluid
- Breast milk (chest milk)
If you test positive for HIV, it is recommended to undergo antiretroviral treatment (ART). ART is a daily medication taken orally that reduces the amount of virus in the body. Without HIV treatment, a person’s immune system can become too weak to fight off serious illnesses and can develop into AIDS (acquired immunodeficiency syndrome).
A person living with HIV who is on antiretroviral treatment and has had undetectable virus levels (a viral load of less than 200 copies/ml of blood) for at least six months cannot sexually transmit HIV to others. People living with HIV who are diagnosed early and receive proper care, treatment, and support can live long, healthy, and fulfilling lives. It’s important to share the public health message that Undetectable = Untransmittable. U=U!
PrEP
Pre-exposure prophylaxis, or PrEP, refers to a medication taken to significantly reduce the chance of HIV developing in your body. Prophylaxis is just a fancy word for disease prevention. PrEP includes daily oral medications, as well as long-acting injectable medication. There are forms of PrEP that can be received at a lower cost. This medication must be prescribed by a medical doctor or nurse practitioner.
There are two pills approved for daily use as PrEP. They are combinations of two anti-HIV drugs in a single pill:
- Truvada® (emtricitabine/tenofovir disoproxil fumarate) is for all people at risk for HIV through sex or injection drug use.
- Descovy® (emtricitabine/tenofovir/alafenamide) is for sexually active cis men and transgender women at risk of getting HIV.
- Descovy® is not marketed towards people assigned female at birth who are at risk for HIV through receptive vaginal sex. This is because people assigned female at birth were not included in the clinical studies used to get this medication approved.
- These pills can be taken “on demand” via the 2-1-1 method, which involves the following:
- Two pills between 2-24 hours before sex
- One pill the day after
- One pill two days after
- This 2-1-1 method provides protection against HIV development (86%), but not as much as daily PrEP.
- This may help reduce the cost of preventing HIV by reducing the total amount of pills taken in a given period.
- The 2-1-1 method may be more suitable for people who are spontaneous and/or forgetful.
A long-acting injectable form of PrEP has also been approved by Health Canada:
- Apretude® (cabotegravir) is approved in Canada for people at risk of HIV through sex. It’s an injection given by your healthcare provider every other month instead of oral pills.
- This may be a great option for people who don’t want to take oral medications, forget to take oral medications, or can’t take oral medications.
- These long-acting doses can be helpful when traveling.
Doxy-PEP
Doxycycline post-exposure prophylaxis, or doxy-PEP, is an antibiotic pill you take after barrier-free sex that can help prevent syphilis, chlamydia, and to a lesser extent, gonorrhea. It’s typically taken within 24 hours of barrier-free sex, but can be taken up to 72 hours after. A good way to remember is the 3-2-1 rule: use it within three days of barrier-free sex, take two-hundred milligrams of doxy-PEP (typically two capsules), and do that once per day.
Current evidence indicates that doxy-PEP is only effective for trans women and people assigned male at birth.
You can learn more about doxy-PEP here: Doxy-PEP: medication to prevent syphilis, chlamydia, and gonorrhea
STBBI Testing, Prevention, & Treatment
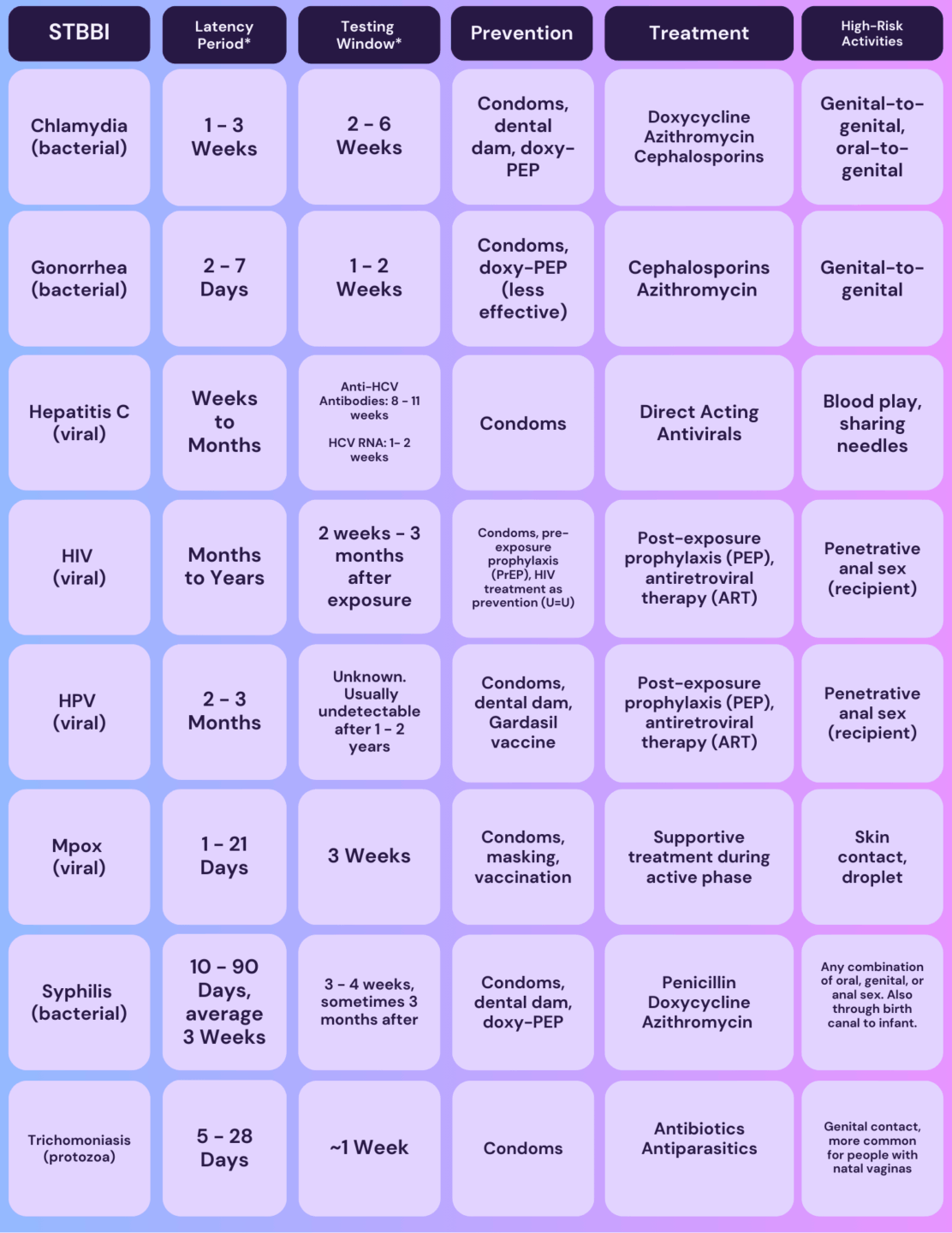
*Latency Period: This refers to the period of time when symptoms may typically begin to present. It is important to consider that the presentation of symptoms may vary and may not present at all despite infection occuring.
*Testing Window: This refers to the period of time between the onset of an infection and when it is detectable on a test. For HIV in particular, the window period varies significantly. Routine testing (every 3-6 months) can help offer results with more certainty.


